AI and Automation in Clinical Evaluation Reports (CERs): From Burden to Breakthrough
How Large Portfolios Can Stay Audit-Ready with Correct, Continuous, and Consistent CER Maintenance
08 Jan, 2026
For medical device manufacturers managing large and diverse portfolios, the real challenge is no longer producing individual CERs. The challenge is maintaining them – accurately, consistently, and on time.
With renewal deadlines approaching under the EU MDR and IVDR, manufacturers must shift to a continuous maintenance model that keeps every CER aligned with current evidence, emerging safety signals, and evolving Notified Body expectations.
Unlike CER development—which focuses on building a strong evidence foundation – CER maintenance is about operational discipline, risk-based planning, and portfolio-wide synchronization. This requires a different set of tools and strategies altogether.
Why CER Maintenance Will Become More Intensive in 2026
Renewal cycles demand fully updated CERs
When Notified Bodies reopen technical files for renewal, there is a growing expectation that CERs demonstrate continuity of clinical evidence. Outdated or partially updated CERs, or CERs that do not follow the established best practices such as a systematic literature review conducted according to relevant guidance documents, evaluation of the relevancy of acceptance criteria, evidence on similar devices, and appropriate scientific justifications can result in major audit findings. Even small inconsistencies accumulate over time and become major obstacles during renewal reviews, causing significant delays in certification and market access.
Large portfolios inherently create scale challenges
The clinical evaluation documents are no longer a compilation of data. The notified body reviewer looks for traceability and consistency across various Plans and Reports, scientific depth, rigor, and validated critical interpretations and conclusions. Increased expectations of clinical evidence from multiple data sources including PMCF, quantitative in-depth analysis, and clear, organized presentation of evidence are not easy to meet for organizations with 50, 100, or 200+ devices constantly in a maintenance cycle. Without structured systems, teams of highly qualified experts spend months managing documents, tracking timelines, and responding to the same notified body questions across multiple CERs.
Maintenance requires systems – not just skill.
Key Challenges Slowing Down Portfolio-Wide CER Maintenance
Outdated State of the Art
The State of the Art must be updated. Because SoTA evolves continuously, infrequent updates lead to:
- Inconsistency across similar device portfolio
- Misalignment with current literature
- Weak comparative analyses
Annual update frequency – challenging timelines
CER maintenance must be coordinated alongside PMS evaluations, PMCF activities, risk file updates, and internal review cycles—involving multiple stakeholders and departments, making timelines difficult to control and predict.
Overlapping evidence across device families
Teams often redo work because CERs for similar devices in the same portfolio use similar content:
- Similar state of the art
- Similar intended use and performance and safety objectives
- Similar testing or preclinical data
- Similar benefit risk profiles
- Overlapping risk content or justifications
Scattered evidence repositories worsen the problem.
How AI Strengthens CER Maintenance Across Large Portfolios
AI-enabled tools are particularly effective during maintenance cycles because they automate repetitive, version-based tasks and provide consistency across device families.
Automated literature refresh cycles
AI tools can:
- Re-run literature searches
- Signal new studies
- Summarize key details
- Compare evidence with prior versions
This ensures evidence stays current without time-intensive manual screening.
Cross-version comparison identifies required updates
AI highlights:
- Changes in clinical evidence
- Variations in safety outcomes
- New regulatory expectations
- Outdated claims or references
Teams update only what has changed—saving time and improving reliability.
Consistency checks across multiple CERs
AI monitors terminology, content alignment, and data presentation to ensure that device families maintain coherent documentation.
Portfolio Priorities for 2026 CER Maintenance
Risk-based annual maintenance calendar
High-risk devices should be prioritized, followed by devices with PMS signals or significant market exposure.
Automated evidence refresh cycles
AI-supported systematic literature search and review allow teams to maintain compliance with comprehensive review of available literature without overburdening resources.
Clear traceability for reviewers
Review outputs with:
- Linked evidence
- Change logs
- Version comparisons
- Structured updates
This reduces internal clarification rounds and creates audit-ready records.
Practical Steps to Stay Audit-Ready
- Start with high-risk and high-volume product lines
Address devices with the greatest regulatory scrutiny or the widest clinical use first. - Introduce planned SoTA refresh cycles
Many manufacturers now refresh SoTA quarterly or bi-annually to stay aligned with evolving technologies and benchmark devices. - Standardize CER formats across the portfolio
Unified templates support:- Efficient, consistent writing
- Reliable and efficient review cycles
- AI-assisted partial drafts with pre-populated content
- Predictable, scalable maintenance workflows.
Organizations that treat portfolio-wide maintenance as strategic portfolio management activity rather than admin work, will be best positioned for renewal success and have shorter time to market than their competitors.
How Celegence Supports Portfolio-Wide CER Maintenance
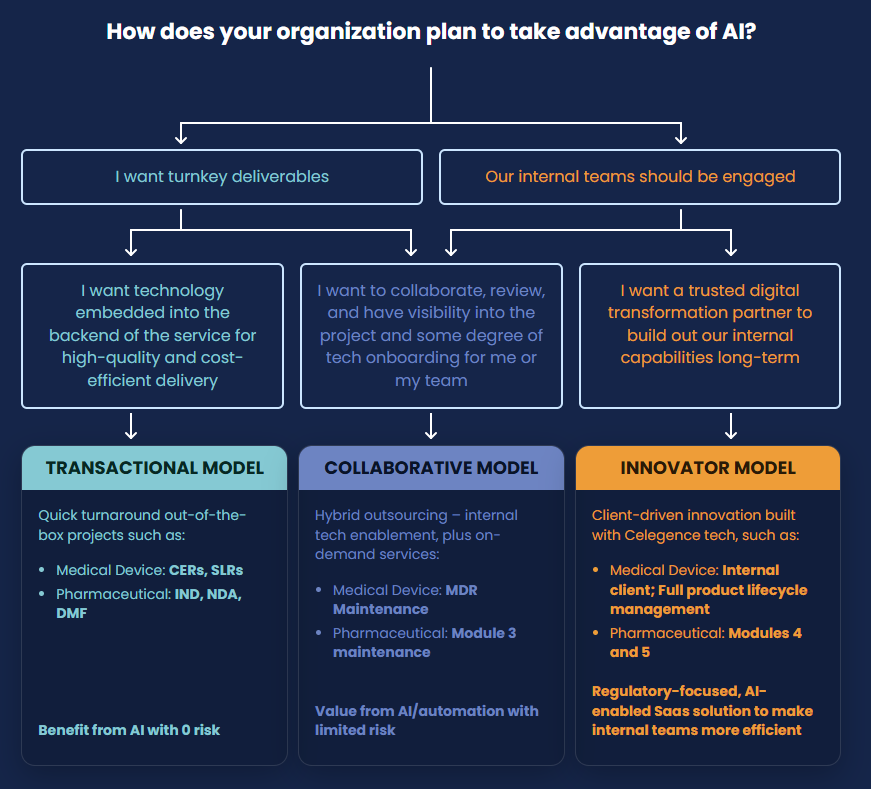
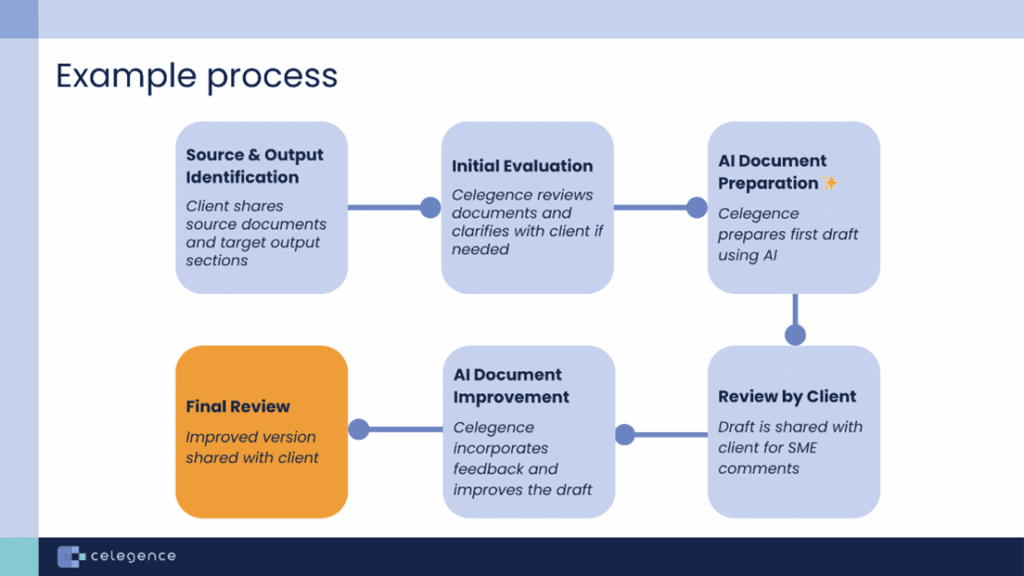
Celegence helps manufacturers implement structured, technology-enabled CER maintenance programs that support annual updates, renewal readiness, and portfolio-wide consistency. With CAPTIS®, our AI-powered authoring platform – teams gain version comparison tools, structured evidence repositories, and automated literature refreshes.
To explore how we can strengthen your CER maintenance strategy, contact us at info@celegence.com.
Other Related Articles
08 Dec, 2025
20 Nov, 2025

11 Nov, 2025

03 Oct, 2025

19 Sep, 2025